
November 13, 2014
Story by Gregory Kennedy; photo by Dale MacMillan
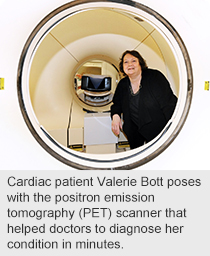
Whenever her mild chest pains and dizzy spells flared up, Valerie Bott found herself having to lie down until her light-headedness passed.
A trip to her family doctor and a swift referral to a specialist soon found her taking part in a major cardiac research project — a smart move that set her right within days.
“Taking part in research is a great idea,” says the 60-year-old Edmontonian. “If they can find what’s wrong faster, of course I’m going to do it. We discovered that part of my heart was not receiving enough oxygen. I’m on medication now and I feel much better.”
 The drug-store supervisor is one of many cardiac patients who are now benefiting from leading-edge diagnosis, shorter hospital visits and reduced exposure to radiation thanks to a clinical research partnership between Alberta Health Services and the University of Alberta’s Faculty of Medicine and Dentistry that provides the only heart imaging of its kind in Western Canada.
The drug-store supervisor is one of many cardiac patients who are now benefiting from leading-edge diagnosis, shorter hospital visits and reduced exposure to radiation thanks to a clinical research partnership between Alberta Health Services and the University of Alberta’s Faculty of Medicine and Dentistry that provides the only heart imaging of its kind in Western Canada.
The Cardiac PET Clinical Research Program uses a positron emission tomography (PET) scanner — a special camera funded by the University Hospital Foundation — to take a circulatory snapshot that looks for poor blood flow, tissue damage or disease in the heart.
Overseeing the program is an interdisciplinary team of doctors from the Mazankowski Alberta Heart Institute and the Nuclear Medicine department at the University of Alberta Hospital.
While PET technology has been around for decades, the new aspect of this research is the injection of rubidium, a radioactive element, into the patient’s circulatory system. There, it acts as a radiotracer, which enables the scanner to ‘see’ the structure and blood flow in the heart.
“It’s a way to assess the heart’s metabolism; how much blood supply is getting through to the various areas of the heart muscle,” says cardiologist Dr. Lucille Lalonde, an Associate Professor of Cardiology at the U of A.
“It can show whether blood supply to an area of the heart muscle is reduced, most often because there’s a narrowing in that coronary artery, which can cause angina or a heart attack.”
Radiologist Dr. Jonathan Abele, also an Assistant Professor of Radiology & Diagnostic Imaging at the U of A, adds: “In angiography, you’re basically taking pictures of the big arteries, the pipes that provide blood flow to the heart. What we’re imaging is what actually flows out the other end. We’re measuring the actual blood flow as opposed to size of the pipe.”
This rubidium-based scan takes an hour, with less than a third of the radiation exposure of patients who undergo a MIBI scan — the current imaging strategy which takes four hours over two trips to hospital, and employs a gamma camera and a radioactive isotope of technetium.
The half-life of rubidium is 76 seconds — which means it decays swiftly and loses half of its radioactivity in barely more than a minute — compared to about six hours for technetium.
“Literally, six minutes after we’ve injected rubidium, there’s virtually no radiation left in the patient,” says Dr. Abele. “MIBI is also a safe procedure but we always try to give the least amount of radiation.”
Both MIBI and PET scans can help doctors determine whether the patient has heart disease, but the newer procedure offers a better alternative for many complex cardiac patients who require more clarity than can be provided by the usual MIBI scan, says Dr. Lalonde.
Both MIBI and PET scans help physicians determine if a patient is at low-risk of having a heart attack in the next two years and could be treated using medical or drug therapy, or if a patient is at high-risk and needs a stent or coronary bypass surgery.
To date, more than 2,000 AHS patients have undergone rubidium PET scans over the past three years, at a rate of about 15 a week, as the research prepares to enter its second phase, evaluating the tubing used to deliver the injection.
“We expect that within a year this procedure will be fully approved in Canada to use outside of research,” says Dr. Abele.