
October 9, 2014
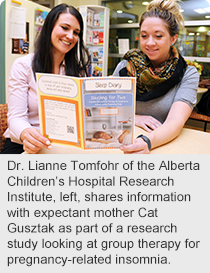
Story by Greg Harris; photo by Paul Rotzinger
For Cat Gusztak, getting enough sleep during her pregnancy once seemed like a nearly insurmountable challenge.
“I would experience a lot of anxiety before bed, or wake up several times during the night and then not be able to get back to sleep,” says Gusztak, who is expecting her first child later this month.
“Initially, I thought it was just due to hormones and all the physical changes taking place.”
 More than simply an inconvenience, insomnia during pregnancy can put women at increased risk for postpartum depression and increase the possibility their newborn will inherit similarly disturbed sleep patterns.
More than simply an inconvenience, insomnia during pregnancy can put women at increased risk for postpartum depression and increase the possibility their newborn will inherit similarly disturbed sleep patterns.
Now, a researcher with the Alberta Children’s Hospital Research Institute is studying a form of therapy to help pregnant women get the restful sleep they need.
“Cognitive behaviour therapy is the gold standard for helping people with insomnia,” says Dr. Lianne Tomfohr, who also holds the Alberta Children’s Hospital Foundation Professorship in Child Psychology.
“In our pilot study, we’re teaching women how to challenge some of the negative thinking they’ve had about sleep, and assessing how effective the approach is in a group setting.”
For example, people with sleep difficulties often overestimate the consequences of spending a night tossing and turning, which cognitive behaviour therapy invites them to challenge.
“People tend to think the next day will be ruined but generally their performance isn’t going to suffer that much,” Dr. Tomfohr says.
At the same time, women in the group learn how to maintain good “sleep hygiene,” which includes a set of habits such as avoiding coffee after noon, keeping computers and televisions out of the bedroom, and not giving in to the temptation to nap during the day.
Although there are sedatives available that are safe for pregnant women to take, many women prefer to try a non-pharmaceutical solution first, Tomfohr says.
About half of pregnant women experience some difficulties sleeping during pregnancy, which tends to worsen during its latter stages. By comparison, about 10 to 15 per cent of the general population struggle with insomnia.
The risk of developing postpartum depression is significantly higher for women with insomnia during pregnancy. Postpartum depression is a type of major depression that can include symptoms such as sadness, hopelessness, irritability and losing interest in things that used to bring joy. It can greatly complicate the task of looking after a baby.
Aside from the increased risk of postpartum depression, Tomfohr says women with insomnia also risk a labour that starts earlier, lasts longer and is more painful.
During the seven-week study, which is supported by community donations through the Alberta Children’s Hospital Foundation, participants first complete a series of questionnaires and have their sleep assessed by wearing a wristwatch-like device that estimates sleep activity. Over the next five weeks, they participate in a once-weekly group therapy session, followed by one week of followup.
Gusztak, one of the early participants in the study, says she’s been amazed by how much her sleep has improved.
“For me a big thing was using electronics in bed. I would wake up and check my phone and sometimes stay in bed for a couple of hours in the morning after I woke up. But now I feel much more rested – and I’m not as irritable,” she says.
To learn more about the study or find out how to participate, contact the study co-ordinator at hearts@ucalgary.ca, or phone 403-220-7595 or see
http://psyc.ucalgary.ca/healthyhearts/current-research.