
February 7, 2017
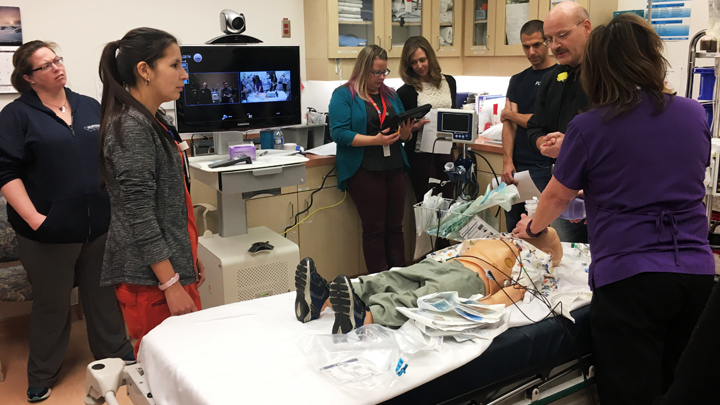
The Stollery PICU Transport Team participates in a mobile simulation with frontline emergency staff at the Peace River Community Health Centre.
Story by Sharman Hnatiuk; photo by Brittany Munce
In a remote northern hospital, EMS brings in a child who has been crushed under a garage door. He has spinal injuries, is in increasing respiratory distress, and is bleeding into the abdomen.
The next steps are crucial in caring for this patient, who will require a medevac to the Stollery Children’s Hospital for advanced treatment.
Luckily, it’s a mock scenario, one of several storylines involving critically ill or injured children. The simulations are part of a new mobile education program with the Stollery pediatric intensive care (PICU) transport team.
It’s offered to acute care, emergency, and ground EMS staff in health centres across northern Alberta to help with the transition of care of critical young patients.
Brittany Munce, a registered nurse with the PICU Transport Team, is leading the charge to bring mobile simulation support to rural healthcare centres that refer patients to the Stollery for advanced care. Along with an intensive care physician and a respiratory therapist, Munce is flying to rural centres to offer specialized pediatric education.
“Our goal is to build a relationship with colleagues at our referral centres so they have the confidence to call the PICU with their questions. This way, we support them in caring for the kids until the transport team can get there,” Munce explains. “It is a great opportunity for us to collaborate with staff throughout our catchment area who have limited exposure to pediatric intensive care patients.”
As a rural physician, Dr. Reena Hansen valued the opportunity to have a PICU team come to Peace River.
“The mobile simulation provided excellent hands-on practice,” Dr. Hansen says. “It was a valuable opportunity for both the PICU team and our rural team to understand the resources available on both sides that will allow us to collaborate better in the future.”
In addition to the simulation of the child injured by a garage door, four other scenarios included a child in septic shock, a child with seizures, a child in respiratory failure, and a child fading in and out of consciousness. In each case, the goal for staff was to recognize medical causes and to decide on treatment steps prior to transportation to the Stollery.
Since April, the PICU transport team has provided education simulation in Fort McMurray’s Northern Lights Regional Health Care Centre, Grande Prairie’s Queen Elizabeth II Hospital, the Fort Vermillion Community Health Centre, High Level’s Northwest Health Centre, and the Peace River Community Health Centre. The response on the education days has been overwhelmingly positive with healthcare sites requesting additional simulation and training support.
“It is incredible to see how just one day with our critical care team has helped to build confidence of our colleagues in remote areas around the province,” Munce says. “It is a great example of a frontline initiative improving the patient and provider experience.”
The PICU Transport Team education initiative is supported with $11,000 from the Stollery Children’s Hospital Foundation.