
November 30, 2012
Story by Greg Harris, photo by Paul Rotzinger
When Jouhar Ali and his wife Alia returned home to Portage La Prairie from Winnipeg last August after the birth of their daughter, everything seemed fine.
 “Nazdana was sleeping, crying and feeding – there were no problems,” Jouhar recalls of the newborn.
“Nazdana was sleeping, crying and feeding – there were no problems,” Jouhar recalls of the newborn.
Then, after a couple of days at home, things took a turn for the worse.
“She wasn’t waking up to feed; we knew there something wrong,” he says.
The infant was taken to hospital in Portage La Prairie, then transferred back to Winnipeg where she was diagnosed with a urea cycle disorder (UCD), a rare genetic condition that can cause a life-threatening buildup of ammonia in the brain.
Ammonia is naturally produced as the body uses protein but, for those with UCDs, the process of converting ammonia to urea (a harmless substance that gives urine its yellow colour) does not work properly.
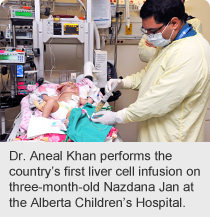
Today, three-month-old Nazdana is part of medical history as the first patient in Canada to receive an experimental and potentially life-saving form of therapy to improve the function of her liver.
Physicians at Alberta Children’s Hospital, led by medical geneticist Dr. Aneal Khan, successfully completed a series of liver cell transplants on Nazdana earlier this month. The long-term stabilization of ammonia levels resulting from the liver cell infusion buys children time until a matching liver can be found and transplanted.
“We have been monitoring Nazdana closely and are happy to report that she has tolerated the liver cell transplant well,” says Dr. Khan, who is also an assistant professor of medical genetics and pediatrics at the University of Calgary, and a member of the U of C-AHS Alberta Children’s Hospital Research Institute for Child and Maternal Health.
“This could represent a big leap forward in managing these cases,” Dr. Khan says. “It’s a promising new bridge therapy that could improve the odds of Nazdana surviving until she is able to undergo a liver transplant.”
To date the procedure has been performed in Germany, including an operation on a Canadian baby, and in a handful of centres in the U.S.
The condition is incurable and very rare: Alberta Children’s Hospital treats about two children with a UCD per year. In Canada, about 50 babies are born annually with the condition.
Without conventional treatment, most newborns with a UCD die within the first two weeks of life. Special medications and a protein-restricted diet improve survival rates but the brain remains exposed to high ammonia levels and even children who survive have a high risk of brain damage. The only long-term treatment is a liver transplant but a transplant in a small child has less chance of success and there is limited availability of organs.
Nazdana’s procedures took place over six days in November at Alberta Children’s Hospital, with each infusion taking about an hour. It is part of a research trial sponsored by the biotechnology firm Cytonet LLC, which covered all costs for the procedures, hospitalizations, blood tests and related expenses. Through a complex process, Cytonet transforms liver cells from donor organs that would otherwise go to waste into cells that can be transplanted.
Nazdana’s father is grateful for the care his daughter has received.
“The health care people – the nurses and the doctors – they have all been outstanding. I have no words to explain it,” says Jouhar.